Kaiser Permanente Bernard J. Tyson School of Medicine (KPSOM) celebrated the scholarly accomplishments of its Class of 2026 students on October 20 during the school’s third annual Student Scholarship Symposium. The event highlighted the culmination of three years of research and inquiry, bringing together students, faculty, and guests to explore projects addressing some of today’s most pressing medical and public health issues.
“The expansiveness of the projects is impressive,” said KPSOM Dean and CEO John L. Dalrymple, MD. “The topic areas, the depth of research, the types of research, how they put it all together, and more importantly, its relevance to real current issues that our patients face. This is just our third time having this event and to see it come to fruition yet again speaks volumes about our students. And without mentorship, we would not be able to actually conduct research like this and to help grow that skill set competency for our students. So I'm thrilled with our faculty and their role as mentors and I think it represents who we are as a school.”
Held in the Medical Education Building lobby, the symposium featured poster presentations allowing students to discuss their findings directly with faculty mentors, peers, and visiting researchers from Kaiser Permanente. Topics ranged from medical education and chronic disease management to digital health tools and health equity.
Jonathan A. Finkelstein, MD, MPH, Senior Associate Dean for Research and Scholarship, commended the students for their perseverance and focus. In his opening remarks, he emphasized how the projects began with patients and community needs rather than pre-set academic interests. He praised the class for applying rigorous ethical and research standards even with limited resources. “You learned to do that,” he noted, “with complete attention to ethical standards, patient privacy, understanding the role of the Institutional Review Board, and non-extractive partnerships in the community.”
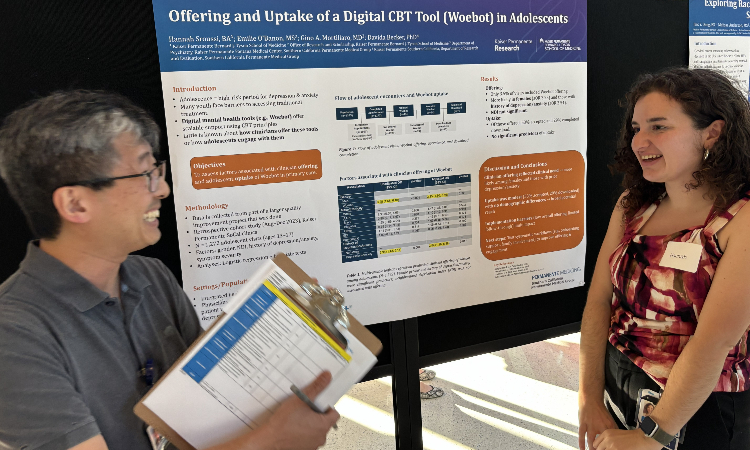
Student Hannah Sroussi’s project, “Offering and Uptake of a Digital CBT Tool (Woebot) in Adolescents,” explored how effectively a chatbot-based mental health app is reaching youth. Woebot uses artificial intelligence grounded in cognitive behavioral therapy (CBT) principles to assist users in managing anxiety and depression symptoms.
Sroussi’s analysis revealed that while physicians were more likely to offer the app to adolescent girls and those with a history of anxiety or depression, actual usage remained low. “We found the roadblock has a lot to do with bridging the communication gaps between adolescents and physicians, and difficulties historically in getting adolescents to adopt new health tools,” Sroussi explained. “For the next steps, [we want to] examine the systemic workflow, see if there’s ways to streamline the process and make it easier for clinicians. They’re offering the app more to women and people with a history of depression and anxiety. Why is that?”
Student Daniel Burke’s study, “Malignancy Risk Stratification of Bethesda IV Thyroid Nodules” focused on thyroid lesions that cannot be easily classified as benign or malignant through biopsy. Burke’s team reviewed seven years of data from more than 400 Kaiser Permanente Southern California members, seeking patterns in ultrasound features and genetic screening (ThyGenX) that might better predict which nodules were cancerous.
The study found ultrasound imaging remained a strong predictor of malignancy, while the use of ThyGenX genetic testing was inconsistent and limited. “The occurrence of these indeterminate thyroid nodules in the general population is very low,” Burke said. “Being able to work with a large data set [at Kaiser Permanente] really helps with picking out some of these features and trends.” Burke and his team plan to expand their work by integrating standardized thyroid ultrasound scoring systems and increasing the use of genetic testing to refine cancer risk models.