
An Ideal Match: Students Trained in Team-Based, Person-Centered Care
Kaiser Permanente Bernard J. Tyson School of Medicine (KPSOM) thoroughly prepares graduates for the challenges that come with residency. Our school is designed to create outstanding clinicians and transformative leaders, and to promote use of cutting-edge technology, a dynamic exchange of ideas, and student well-being. KPSOM teaches students to be resilient, reliable champions of the patients and communities they serve. They learn to practice person-centered care, to appreciate the many factors that influence health, and to understand and meet the needs of people from all backgrounds. Taught and mentored by leaders in a small-group, collaborative approach, they study the entire healthcare system and how it interacts with patients.
KPSOM's innovative curriculum is preparing students to embark on a range of career paths – and to be outstanding clinicians.
Setting KPSOM Apart
Our Students
- Highly selective medical school with lowest admission rate in the US.
- Approximately 50 students per cohort.
Our Training
- Students begin seeing patients in outpatient clinics, with support from a team of healthcare professionals, at beginning of first year.
- Small-group, in-person, case-based active learning heavily leveraging early and frequent high fidelity and standardized patient simulation for teaching and assessment.
- Spiral approach revisits and builds on scientific concepts over the entire four years.
- Longitudinal integrated clerkship model, with Family Medicine/Internal Medicine beginning in Year 1, followed in Year 2 by six core clerkships (Emergency Medicine, Family/Internal Medicine, Obstetrics and Gynecology, Pediatrics, Psychiatry, and Surgery).
- Two academic years of advanced clinical rotations and electives inside and outside Kaiser Permanente prepare students to have an impact wherever they pursue graduate medical education, and beyond.
- At least three clinical selectives (sub-internship experiences) in the third year, in which students have intern-like responsibility for patient care, with appropriate supervision.
- A community-based medicine rotation as well as other clinical and non-clinical experiences outside of the Kaiser Permanente health care system.
- Longitudinal physician coaching program supports health and well-being, resiliency skills, development of a growth mindset, and development of a professional identity.
Our Curriculum
- Competency-based medical education prioritizing skills required for excellent clinical care.
- Integrated curriculum with strong focus on health systems science, the science of how human relationships, organized in systems, influence health.
- Four longitudinal threads woven across the four-year program: Advocacy and Leadership; Inclusive Practice; Health Promotion; and Interprofessional Collaboration.
- Anatomy taught in a case-based longitudinal format utilizing pre-dissected plastinated cadavers and various computer-assisted technologies, including augmented reality and simulated diagnostic imaging instrumentation.

LICs: Real Experience With Patients, From the Start
At KPSOM, from the beginning of medical school, students participate in patient care through the Longitudinal Integrated Clerkship (LIC). Under the guidance of a one-on-one physician-preceptor in Family Medicine or Internal Medicine, they collaborate with physicians, nurses, pharmacists, social workers, and others in caring for a panel of patients one half day per week in their first year. In the second year, students continue their Family Medicine/Internal Medicine clerkship with the same preceptor and patients, and complete longitudinal clerkships in Emergency Medicine, Obstetrics-Gynecology, Pediatrics, Psychiatry, and Surgery, including inpatient immersion experiences.
LICs enable students to build relationships with patients over time, because they may see them over a two-year period. Through interactions with their physician-preceptor’s healthcare team, students experience the flow of a medical practice and the value of interprofessional communication in enabling safer, more effective care. From day one, students practice content taught in their doctoring course.
In Years 3 and 4, students complete their sub-internships or selectives in Advanced Medicine, Critical Care, and their chosen specialty. They also complete a community medicine rotation in an external setting, such as a Federally Qualified Health Center (FQHC), or prison health setting. Students must complete an additional 16 weeks of clinical electives. KPSOM offers over 140 clinical electives, and most clinical selectives and electives take place at Kaiser Permanente residency and fellowship teaching sites, though students have affiliated electives available to them at other local institutions, including UCLA David Geffen School of Medicine, USC Keck School of Medicine, and Cedars-Sinai Medical Center.
By graduation, students have four full years of experience managing patients, working with electronic health records and other technology systems, and applying their medical knowledge holistically – skills that will help them transition to the responsibilities and challenges of residency. Our capstone Residency Immersive course provides additional preparation for practice in their chosen specialty.
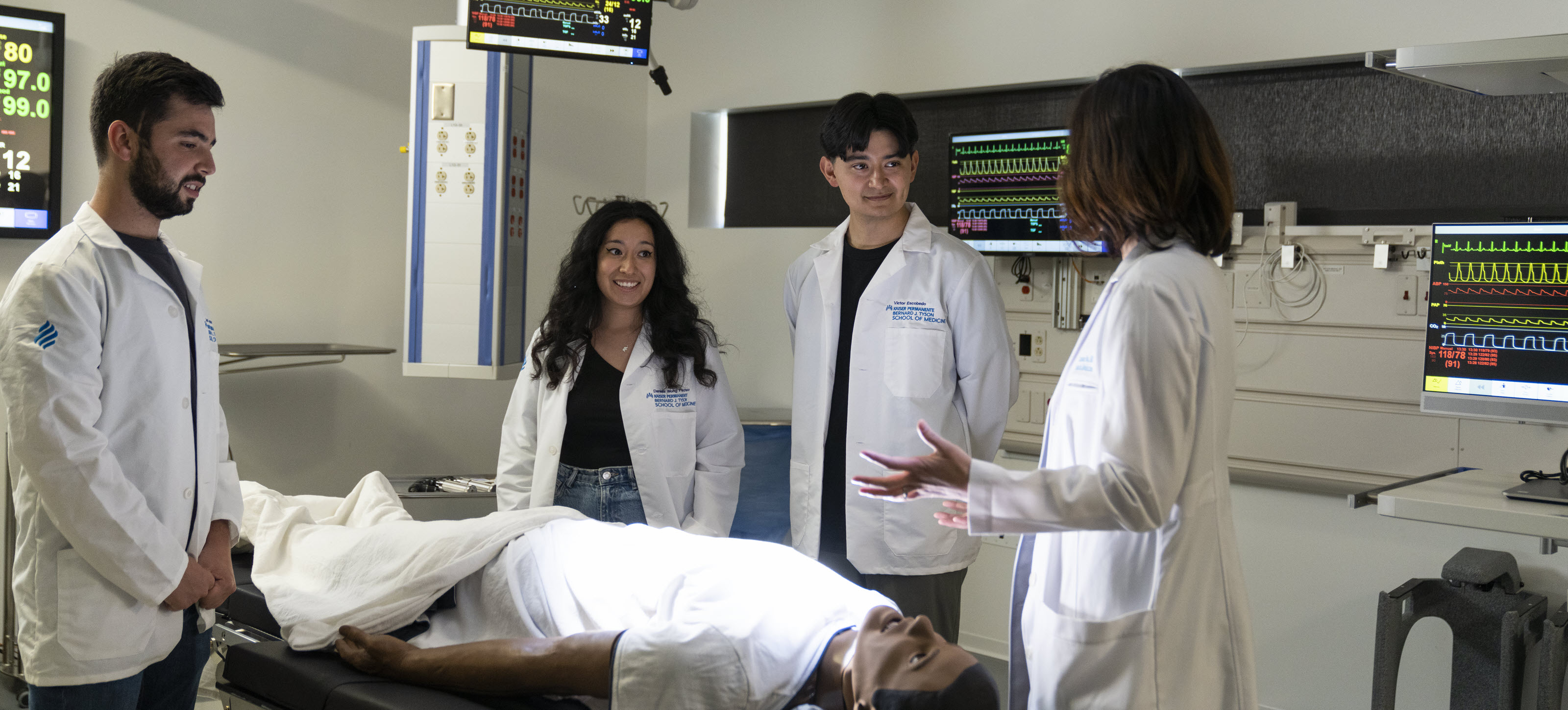
Simulation Center: Building Skills and Confidence for Doctoring
From the first weeks of medical school and across all four years, KPSOM’s robust simulation curriculum prepares students to deliver effective, patient-centered care in a safe learning environment and provides opportunities to learn and practice foundational skills across a wide range of scenarios.
Our Simulation Center provides access to state-of-the-art technology that replicates a real clinical setting as closely as possible, including use of electronic health records and point-of-care ultrasound. Working with standardized patients, students practice diverse tasks, from taking hypothesis-driven histories and physical examinations to applying advanced communication skills and engaging in interprofessional collaboration. High-fidelity mannequins enable the learning of emergent care, crisis management, and teamwork, while task trainers are used to practice the psychomotor skills necessary for complex procedures. During their first two years, students are concurrently enrolled in Integrated Sciences courses that teach Doctoring skills and use patient cases to integrate core knowledge from the three pillars of the school curriculum (Biomedical Science, Clinical Science, and Health Systems Science) and the four longitudinal threads.
Simulation-based assessments are a significant part of KPSOM’s overall assessment program. In addition to participating in objective structured clinical examinations (OSCEs), students engage in a longitudinal Progress OSCE. This format presents students with the same graduation-level cases once per year, allowing direct comparison of performance over time. These cases assess multiple competencies, including communication in difficult settings, interprofessional teamwork, telemedicine, inclusive behavior, and ethical reasoning, providing a holistic picture of each student’s clinical skills. Throughout these experiences, students become accustomed to receiving constructive feedback and incorporating it into their practice.
Health Systems Science: Putting Care in Context
Instead of a traditional approach – lectures in basic sciences for the first two years, clinical sciences the third and fourth years – KPSOM students are immersed in biomedical science, clinical science, and a third discipline, health systems science, which explores how human relationships influence health, across all four years.
This emphasis on not just the doctor-patient relationship but also the function and performance of the entire healthcare system – care teams, hospitals, insurance, families, workplaces, schools, communities, policies, the justice system, the environment, and more – gives KPSOM students a wider perspective and valuable skills in patient safety, performance improvement, quality improvement, and systems-based practice. By the time they graduate, students have had a minimum of eight weeks of sub-internship experience working on care delivery teams with residents within Kaiser Permanente’s integrated healthcare system. This training includes working with residents and practicing interprofessional communication with students from other health professional schools and healthcare systems and environments.

Coaching for Professional Development and Personal Well-Being
KPSOM students don’t go it alone. They are supported throughout the four-year program by physician-coaches who help them maximize their potential in the clinical setting and balance their professional and personal life.
The school’s competency-based education program helps students acquire skills needed to excel as clinicians. Physician-coaches work with students to address any gaps in learning, supporting ongoing performance improvement, and helping further a growth mindset and commitment to lifelong learning.
Through a course called REACH (Reflection, Education, Assessment, Coaching, and Health and well-being), students are paired for all four years with a physician-coach, meeting regularly one-on-one with their coach as well as in small group sessions that provide guidance and support for their professional identity formation, personal well-being and resilience, to maximize performance and reduce the risk of burnout during medical school and beyond.
Future Doctors, Future Leaders: For a Changing Healthcare World
Healthcare and medicine are undergoing constant and rapid change. So, too, is the world changing, challenging us to engage in thoughtful conversations about the multifaceted healthcare issues of an emerging America that is increasingly diverse.
Physicians must adapt and thrive in this evolving environment. At KPSOM, students learn not only to be excellent clinicians but also inspiring leaders – in medicine and in the communities they serve.
Advocacy and leadership development, along with a mission-driven focus on inclusion, are core elements of the KPSOM curriculum. Students have opportunities to hone leadership skills by serving on school committees, participating in community groups, developing a student-run clinic, and more. Through the inclusive curriculum, students focus on bias mitigation, intersectionality, and structural competency as applied to all aspects of healthcare. Through collaboration and small group learning, they build strong ties, preparing them to connect authentically with colleagues and patients of all backgrounds.