A recent case report details the rare occurrence of spinal epidural lipomatosis (SEL)—an abnormal buildup of fat in the spinal canal—in a 1-year-old boy undergoing treatment for medulloblastoma, making him the youngest patient with this condition ever documented. SEL can compress nerves in the spine, potentially causing pain, weakness, or urinary problems, but in this case, the child remained symptom-free throughout. Remarkably, the patient was not obese and had received a much lower cumulative dose of steroids than typically seen in SEL cases, challenging the conventional understanding that obesity and prolonged steroid use are the primary risk factors.
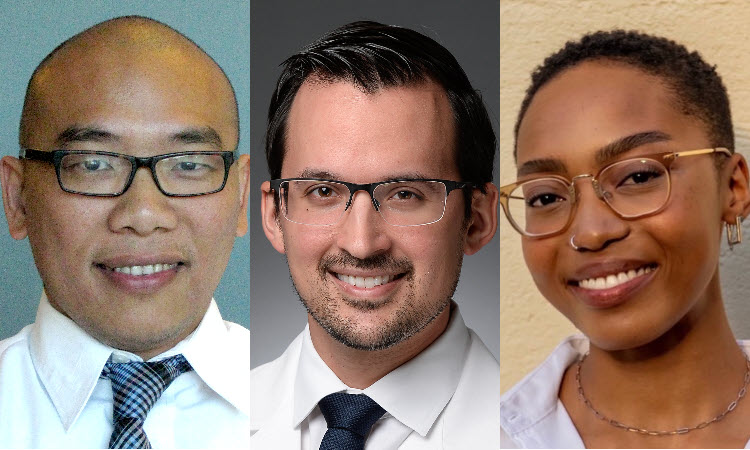
The case report, coauthored by KPSOM faculty members Darian Esfahani, MD, MPH, Assistant Professor of Clinical Science; Hung C. Tran, MD, Clinical Assistant Professor of Clinical Science; and KPSOM student Mandisa Keswa, was published in the peer-reviewed scientific journal Child’s Nervous System. It describes how the child received chemotherapy and autologous stem cell rescue (AuSCR), standard treatments for aggressive pediatric brain tumors. Three months after completing these therapies, MRI scans revealed SEL, and lab tests showed a temporary spike in blood triglyceride levels, a marker of metabolic disturbance. Over the following months, the SEL gradually resolved without surgical intervention or changes to his treatment plan, and the child experienced no neurological complications.
This report is significant because it broadens the understanding of SEL in children with cancer, suggesting that chemotherapy and stem cell rescue—rather than just steroids or obesity—may trigger this rare complication. The authors highlight the need for clinicians to consider SEL when interpreting spinal imaging after such treatments, even in young, non-obese patients with minimal steroid exposure. The findings also raise questions about the underlying metabolic changes caused by cancer therapies and point to the importance of further research to clarify SEL’s causes and optimal management in pediatric oncology.