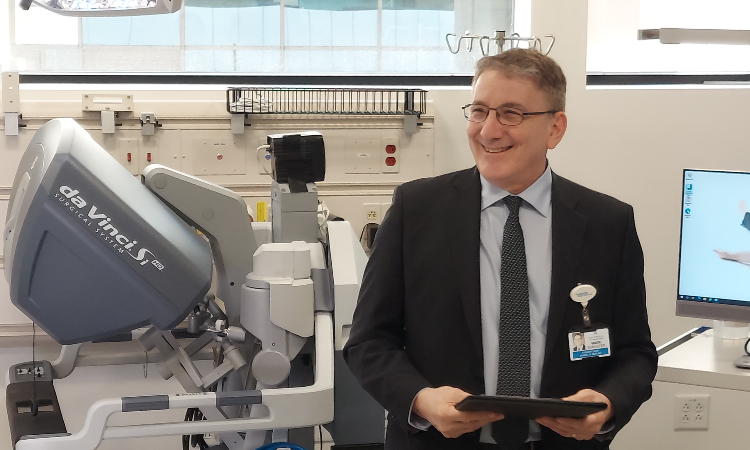
Students at the Kaiser Permanente Bernard J. Tyson School of Medicine (KPSOM) will soon have opportunities to learn minimally invasive robotic surgery techniques, thanks to the donation of a da Vinci Surgical System from Kaiser Permanente West Los Angeles Medical Center.
“The da Vinci robot is a great addition to our school’s Simulation Center, and I can’t thank our West Los Angeles Medical Center enough for this wonderful gift,” said Mark Schuster, MD, PhD, Founding Dean and CEO. “Our students, especially those considering going into surgery, now have another terrific learning tool to use in developing their skills.”
The da Vinci unit arrived at KPSOM in November and is currently in the process of being fully set up. The machine will offer students the opportunity to learn basic robotic surgery techniques, giving them a foundation to continue learning more complex procedures if they choose to pursue residency training in a surgical field where robot-assisted surgery is used in procedures such as nephrectomy, prostatectomy, hysterectomy, cholecystectomy, hernia repair, bowel surgery, and more, school officials said.
The da Vinci unit was in service for approximately 8 years, Kirk Tamaddon, Kaiser Permanente Area Medical Director, said at a recent event commemorating the donation to KPSOM. West Los Angeles Medical Center has been at the leading edge of this technology within the Kaiser Permanente system, becoming the first medical center to perform robotic surgery in 2008, and later, the first to have two robotic surgery machines.