In the project, “Use and Outcomes of Corticosteroid (CS) and Platelet-Rich Plasma (PRP) Injections for Knee Osteoarthritis,” KPSOM student Virginia Xie investigated the controversial use of PRP injections. “There’s a lot of controversial data in terms of the effectiveness of these injections,” Xie said. “And a lot of mixed reviews in terms of how well PRP works and how it compares to more established treatments, like corticosteroids.” In the study, Xie leveraged data from Kaiser Permanente electronic medical records of more than 160,000 patients and developed demographic profiles on who tends to receive PRP therapy. “They tend to be younger, male, white, and higher income, with fewer comorbidities than those who receive steroid. So there seems to be a population of younger, healthier, wealthier patients that are receiving this therapy. “
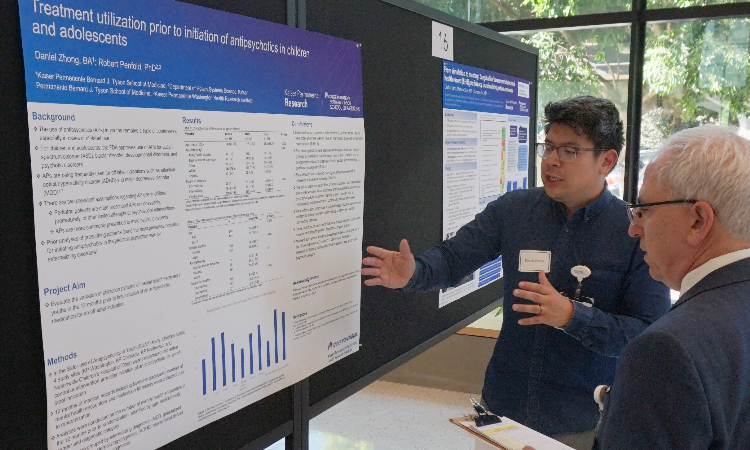
Some projects were informed by personal experiences. KPSOM student Daniel Zhong, a former middle school teacher who also has a background in pharmacy, said he came to medical school with a specific interest in studying adolescent psychiatry. He explored the use of antipsychotic drugs in young persons through the project, “Treatment utilization prior to initiation of antipsychotics in children and adolescents.”
“I’m interested in how things like gender identity, race, ethnicity, as well as types of diagnoses, affect someone’s treatment trajectory, especially the type of care they receive,” Zhong said. “I wanted to dig further into that.” His study’s findings, “suggest that there’s a correlation between some of these demographic categories and the amount of psychotherapy, and the amount of times [patients] see a provider in the twelve months before they start an antipsychotic,” he said.
The event also fostered mentorship and collaboration, as students from other classes interacted with the presenting students, deepening their understanding of the research process, said Jonathan A. Finkelstein, MD, MPH, Senior Associate Dean for Research and Scholarship.
“It’s great to see the buzz in the room,” said Finkelstein. “We have [first-year] students looking at the work of the [fourth-year] students and there’s a kind of intergenerational teaching going on, and there are faculty here, so it’s a great moment for the school. And then, for me, to see some of these projects that were just ideas when the students were in their first year, and now they’re really well done contributions that they’re really proud of, is incredible. Many of them have already been presented at national meetings, and some are going to be published. Every student, I think, has learned something really important about research.”
The following is a complete listing of projects presented at the 2024 KPSOM Student Scholarship Symposium:
Ahmad Alach, “Diagnostic Imaging Utilization Associated with Primary Care Telemedicine and In-Person Visits in a Large Integrated Health System.” Mentor: Peter Huynh.
Amina Ahmed, “Incidence Of Stroke in Pregnant Patients with Cavernous Malformations.” Mentor: Navdeep Sangha.
Anna Richards, “Social factors associated with uptake and satisfaction with a post-hospitalization home-delivered meals benefit in Medicare Advantage.” Mentor: Huong Nguyen.
Ariana Vajdi, “Effects of provider language & racial/ethnic concordance on patient knowledge of HPV and cervical cancer screening.” Mentor: Quyen Ngo-Metzger.
Ariel Silverman, “Associations Between Health Related Social Needs and Total Healthcare Cost in a Large Integrated Delivery Network.” Mentors: Robert Nocon, Paul Chung.
Aya Badran, “Potential Effect of Parental Psychopathology on Adolescent Neurostructural Development.” Mentors: Natalia Orendain, Paul Chung.
Brandon Towns, “Comorbid Alcohol and Cocaine Use Disorder and Adverse Cardiac Outcomes.” Mentors: Cynthia Campbell, Stacy Sterling.
Cara Snead, “Understanding the Relationship Between Social Needs & Cervical Cancer Screening.” Mentor: Quyen Ngo-Metzger.
Caryssa Lim, “School Attendance Following Receipt of Care from a School-Based Health Center.” Mentors: Paul Chung, Rebecca Dudovitz.
Christian Zapp, “School Attendance Following Receipt of Care from a School-Based Health Center+C10+C11.” Mentor: Robert Penfold.
Cristo Carrasco Mendoza, “Incidence of Depression and Anxiety Across Different Racial Groups After Hidradenitis Suppurativa Diagnosis: A Retrospective Cohort Study.” Mentors: Jason Castillo, Anna Davis.
Cruz Riley, “Identifying Predictive Risk Factors for Skin Cancer Development in Solid Organ Transplant Recipients.” Mentors: Linda Tolbert, Annette Adams.
Crystal Chang, “Barriers to medication adherence in young Black and Hispanic patients with uncontrolled hypertension: a qualitative study.” Mentors: Linda Tolbert, Annette Adams.
Daniela Wong Pacheco, “Sex, Socioeconomic Status, and Self-perceived Risk of Opioid Overdose in Patients Prescribed Long Term Opioid Therapy.” Mentor: Ingrid Binswanger.
Daniel Zhong, “Treatment utilization prior to initiation of antipsychotics in children and adolescents.” Mentor: Robert Penfold.
Deshae Gehr, “From simulation to mastery: Longitudinal assessment of electronic health record (EHR) proficiency in a simulated patient encounter.” Mentors: Matthew Silver, Candace Pau.
Hailey Shoemaker, “Training the Next Generation of Physicians in Sub-Saharan Africa: Conflict in International Post-Graduate Medical Education Partnership Programs.” Mentor: Jeffrey Brettler.
Hayden Ngan. “Comparison of ACEs Reporting Between Clinic and Telephone-based Screening.” Mentors: Paul Chung, Rebecca Dudovitz.
Heejeong Kim. “Characterization of Providers Who Complete Postpartum IPV Screenings.” Mentors: Liza Eshilian-Oates, Robert Nocon.
Henry Dong, “A Novel Approach to Increase Outpatient Rehabilitation Utilization Post-stroke.” Mentors: Navdeep Sangha, Bev Green.
Iris Smith, “Risk of preterm birth recurrence in successive pregnancies.” Mentor: Darios Getahun.
Isabella Ramirez, “Racial and ethnic disparities among patients with Multiple Sclerosis before and after implementation of the MS Treatment Optimization program in KPSC.” Mentor: Annette Langer-Gould.
Jacaueline Xu, “How has quality of hospital care changed over time for Medicaid beneficiaries? Analysis of hospitalizations from 2016-2019.” Mentors: Robert Nocon, Paul Chung.
Jacob Abrahams, “Neighborhood Level Socioeconomic Disadvantage and Adherence to Guidelines for Surveillance of Patients with Incidentally Detected Pulmonary Nodules.” Mentor: Michael Gould.
Jacob Gharemani, “Medical Interpretation Services and Total Knee Arthroplasty Outcomes.” Mentors: Ronald Navarro, Elizabeth Paxton.
Jesus Fuentes, “Physician Perceptions on Utilizing Medical Interpreters for Surgical Encounters.” Mentor: Elisabeth McLemore.
Jordan Cornwell, “Relative Risk of Mental Health Diagnoses Following Mild Traumatic Brain Injury.” Mentors: Robert Sallis, Angela Lumba-Brown.
Kaleigh Allen, “Case Management Services for Unhoused Sex Workers: Limitations, Facilitators, and Visions for Improvement.” Mentor: Isabel Chen.
Khush Dhaliwal, “Factors Influencing Civic Engagement in a Grassroots Mutual Aid Group.” Mentor: Gery Ryan.
Kristian Diaz, “Individual- and Neighborhood- level Socioeconomic Characteristics and Prenatal Depression.” Mentor: Lyndsay Avalos.
Maranda Gaines, “Implications From the Experiences of Family Medicine Physicians Through Birth and Death.” Mentor: Gery Ryan.
Mariel Colella, “The Cost of Contamination: Understanding the financial impact of blood culture contamination at Kaiser Permanente Los Angeles Medical Center.” Mentor: Sean Fitzwater.
Maryam Ahmad, “Care Managers' Role in Supporting Caregivers of Persons with Dementia: A Qualitative Study.” Mentor: Huong Nguyen.
May Let Wah, “The Impact of Biologic Therapy on Bowel Resection Rates in Patients with Inflammatory Bowel Disease (IBD) in an Integrated Healthcare System.” Mentor: Elisabeth McLemore.
Michael Chapek, “The Prevalence of Persistent Toe Walking in Children with and without Autism Spectrum Disorder and the Odds of Subsequent Surgery.” Mentor: Jeffrey Kessler.
Michael Langevin, “Rebound in Fecal Testing, Colonoscopy Utilization, and Colorectal Neoplasia Detection During the COVID-19 Pandemic Among Screening-Eligible Patients in a Large Northern California Integrated Health System.” Mentors: Theodore Robert Levin, Christopher Jensen.
Nala Al-Khatib, “Food Insecurity During Pregnancy and Early Developmental Childhood Outcomes.” Mentor: Lisa Croen.
Neipori Pelle, “An analysis of the effect of the COVID-19 pandemic on ED revisits for abdominal complaints.” Mentor: Jonathan Finkelstein.
Olivia Goodman, “Intervention Opportunities, Barriers, and Strengths to Addressing Social Determinants of Health Among Those Facing Housing Instability in Colorado.” Mentor: Morgan Clennin.
Paula Hornstein, “Global Health Training Opportunities During Pediatric Hematology/Oncology Fellowship: Results from a Survey of Program Leaders.” Mentors: Temidayo Fadelu, Jeffrey Brettler.
Priyanka Achalu, “Fertility preservation utilization in an integrated healthcare system: population demographics and barriers to attempting sperm banking.” Mentor: Aravind Chandrashekar.
Saadiq Garba, “Prior Screening for Latent Tuberculosis among Patients Diagnosed with Active Tuberculosis: Missed Opportunities?” Mentor: Sara Tartof.
Shaheed Muhammad, “Self-Reported Screening for Oropharyngeal Sexually Transmitted Infections and History of Past Infection in MSM of the Portland Metro Area.” Mentors: Mark Schmidt, Timothy Menza.
Victor Escobedo, “Disparities In Direct Oral Anticoagulant Orders In Patients With Nonvalvular Atrial Fibrillation Within A Large Integrated Health System.” Mentor: Jaejin An.
Virginia Xie, “Use and Outcomes of Corticosteroid (CS) and Platelet-Rich Plasma (PRP) Injections for Knee Osteoarthritis.” Mentors: Ronald Navarro, Anna Davis.
Wilkin Munoz Orozco, “Early Postpartum Glucose Tolerance Among US-Born versus non-US-Born Women with Gestational Diabetes Mellitus: The SWIFT Study.” Mentor: Erica Gunderson.