Patients and their loved ones may have experienced a few head-scratching moments when a clinician may have inadequately communicated details about a diagnosis, treatment, or medical test, particularly when there is uncertainty in the diagnosis, treatment effects, or testing reliability.
Sadly, there is a dearth of established curricula and dependable assessment methods to educate clinicians on how to appreciate uncertainty in medicine and effectively communicate this information to others, but several Kaiser Permanente Bernard J. Tyson School of Medicine (KPSOM) faculty members are working together to help future medical students improve their overall understanding and communication skills related to uncertainty within the clinical practice space.
Recognizing the need for more education in this area, the ABIM (American Board of Internal Medicine), Gordon and Betty Moore, and Josiah Macy Jr. foundations awarded $360,000 to three groundbreaking projects aimed at helping clinicians communicate about and process uncertainty more effectively, which in turn improves patient-doctor trust. Candace Pau, MD, KPSOM Faculty Director of Simulation and Assistant Professor of Clinical Science, led an effort to find solutions to this pressing issue along with Carla Lupi, MD, FACOG, KPSOM Associate Dean for Assessment and Evaluation and Professor of Clinical Science, and Wendy Madigosky, MD, MSPH, FAAP, KPSOM Interprofessional Collaboration Lead, Education Director, and Associate Professor of Health Systems Science.
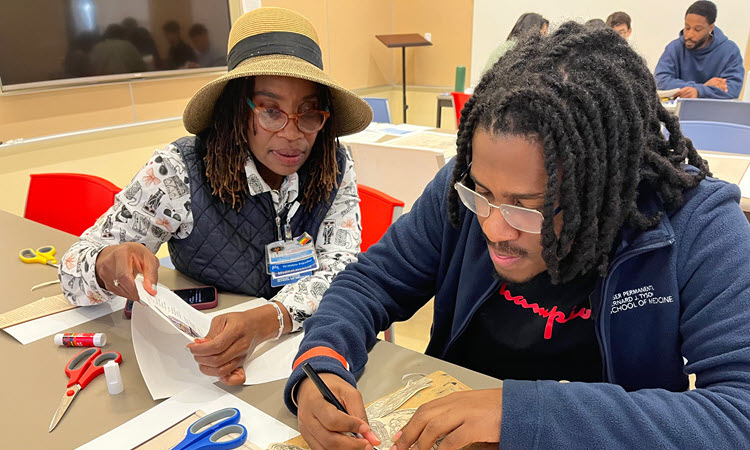
The team of co-investigators received a $120,000 grant from the three foundations to develop a competency-based curriculum to teach learners the skills, knowledge, and attitudes needed to effectively communicate about uncertainty. The grant covers a two-year period from fall 2023 through fall 2025. The team’s project proposal entitled “A competency-based approach to communication of clinical uncertainty within intra- and interprofessional health care teams” includes hands-on learning approaches to help medical students collaborate and communicate with patients and clinicians across interprofessional care teams.
“[The foundations] put out a call looking for specific [curricula] that would help address uncertainty in medicine,” said Pau. “Our proposal was a really good fit … because we already have [learnings on uncertainty] in our curriculum and educational program outcomes.”
Pau further explained that the school curriculum presently incorporates elements such as how to communicate uncertainty and collaborate with patients and their families in times of uncertainty. The co-investigators’ proposal aims to share this existing curriculum and to expand on that curricular work to further develop and more cohesively integrate pieces of the curriculum. Part of that curriculum includes establishing a set of skills, knowledge, and behaviors that tie to the idea of addressing uncertainty through self-directed learning skills, giving and receiving feedback, and interprofessional communication and collaboration.
The potential for miscommunication and/or conflict can increase when working with an interprofessional healthcare team of nurses, pharmacists, doctors, and social workers, so ensuring team alignment and communicating a shared mental model and plan with the patient is key, Pau said. The team’s grant proposal builds on Madigosky’s efforts around KPSOM’s interprofessional collaboration partnership with Western University’s College of Graduate Nursing and the University of Southern California Mann School of Pharmacy. Together, these entities will further their work in developing a curriculum that specifically addresses how to deal with uncertainty within an interprofessional team collaboration setting.
“Interprofessional collaboration is essential when diagnoses, testing, and treatments are uncertain, which occurs regularly with today’s complex healthcare environment,” said Madigosky. “Ensuring that students are skilled in navigating and communicating about uncertainties within the healthcare team will benefit their future colleagues, patients, and [their] families.”
Lupi said she wishes more clinicians had the opportunity to learn about communicating uncertainty to patients and colleagues much earlier. She said creating a comfortable space between patients and their medical teams is an important goal in addition to creating space for clinicians to manage their own negative or challenging internal reactions to uncertainty, which she added can be difficult for early learners.
“A problem with our educational system to date [is that it] has heavily rewarded students for knowing the best answer to a five-option, multiple choice question and so little rewarded them for asking the right questions and then managing the new information and the ongoing uncertainty that comes out of that … we really do need a bit of a paradigm shift,” said Lupi.
Pau believes medicine has shifted from a paternalistic model of care in which the doctor is thought to know the right answer without fail, to more of a focus on what it means to live well and with high-quality care. The KPSOM trio posits that care should be person-centered, collaborative, and communicative in a way that allows clinicians to be honest when they do not know the answer to pressing health questions and can work collaboratively with a patient to make decisions about their health in the face of that uncertainty.
“I think those communication and collaborative skills also contribute a lot to patient health and wellness, and so that's something that hopefully this curriculum will help to contribute to,” said Pau.