Cross-Cultural Exchange
The KPSOM quartet was led by Jeff Brettler, MD, KPSOM Director of Global Health and Assistant Professor of Health Systems Science, who stated the goal of the program is to deepen students’ proficiency in history and physical exam skills, expose students to a different healthcare delivery system they can compare and contrast with US healthcare systems, encourage the development of communication skills, including effective cross-cultural communication, and incorporate cultural humility as an ongoing theme throughout the month-long program.
Dr. Brettler said the students successfully accomplished these objectives while serving as “amazing ambassadors” who “represented the school extremely well” during its first formal experience with the AMPATH consortium. The students’ experience in Eldoret was quite different from what they would experience clinically, culturally, and structurally in the US, including the use of the Kiswahili language and even how health information is obtained. In addition to their time rounding in hospitals and learning in local clinics, KPSOM students were able to bond with their colleagues and Moi medical students whom they invited to IU House—the Eldoret compound where the KPSOM group resided—for lunches and dinners. Some members of the integrated teams also watched soccer matches together and learned more about each other and pressing social issues during weekly fireside chats.
While Dr. Brettler and the students acknowledged the impossibility of learning everything about different cultures, they shared that having cultural humility, or an interest in understanding and appreciating the culture of others, was key in this experience in addition to having flexibility, leaning on and learning from their Kenyan team members, and being a careful observer of cultural norms.
When the KPSOM students were not rounding with their teams, the group was able to coordinate a weekend day trip that included a hike with Dr. Brettler, and students had enough downtime to bond with one another, peers, and even work on residency applications. Fratt said the group really loved being in the lush city of Eldoret and enjoyed spending time at IU House. The group even ventured to Eldoret’s picturesque Torok Falls the week before their cultural exchange began and Fratt described the city as “a fun, beautiful place to be.”
Considering that KPSOM students and global health initiative staff had discussions stateside about cultural humility, Zevallos-Roberts said these discussions also carried over to the AMPATH group. “I think the most important thing is knowing the power and privilege that your status comes with and being very careful about wielding that power.”
“The cultural practices are different, so [our students] really … have to learn everything through all of those different aspects,” Dr. Brettler added. “The biggest learnings [were] around approach to clinical diagnosis and management when you don't have all of the resources that you have in a high-resource setting like the United States, so there is increased emphasis on history and physical exam. There is [an] increased emphasis on creating a differential diagnosis based upon much more limited information than you would in a setting like the United States, so it really expands [the students’] thought process[es] and their actual way of approaching clinical problems.”
Partnership and Bidirectional Exchanges
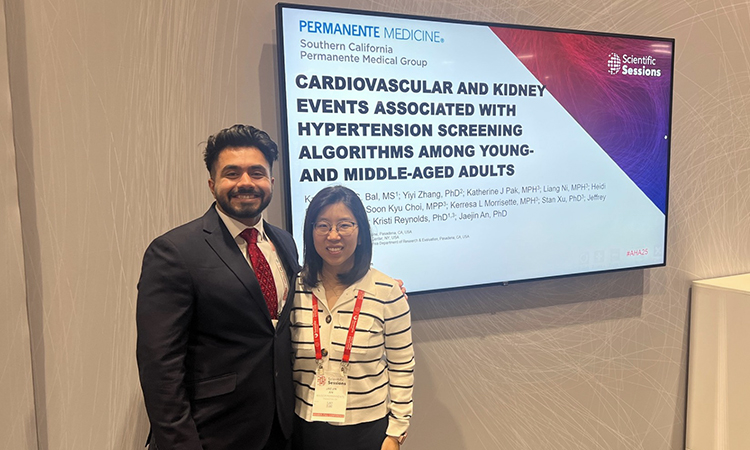
The Global Health Office’s mission philosophy is a tripartite approach that includes the training of clinicians, clinical care collaboration, and research. KPSOM and AMPATH aim to ensure those components are bidirectional with benefit to both participating parties, which is why KPSOM plans to bring its students to Kenya annually and is committed to hosting and facilitating the training of Kenyan medical students on KPSOM’s campus in the very near future; this is a goal the global health initiative team is actively working toward.
As students took part in their rotations, Dr. Brettler was involved in many other aspects of the Eldoret cultural exchange. For instance, he met with AMPATH faculty and staff to develop relationships to begin clinical work in population health around hypertension and chronic disease management, an area of personal interest. This area of focus is particularly key due to the country’s under-resourced nature and lack of significant health infrastructure outside of its emphasis on HIV and AIDS. Dr. Brettler and KPSOM students also spent time in the HIV clinic where there is a need to integrate chronic disease into HIV care, a project Dr. Brettler is looking forward to tackling. The aim of these efforts was to better understand workflows, the clinic’s electronic system, what kind of data was collected, and how the teams could work collaboratively.