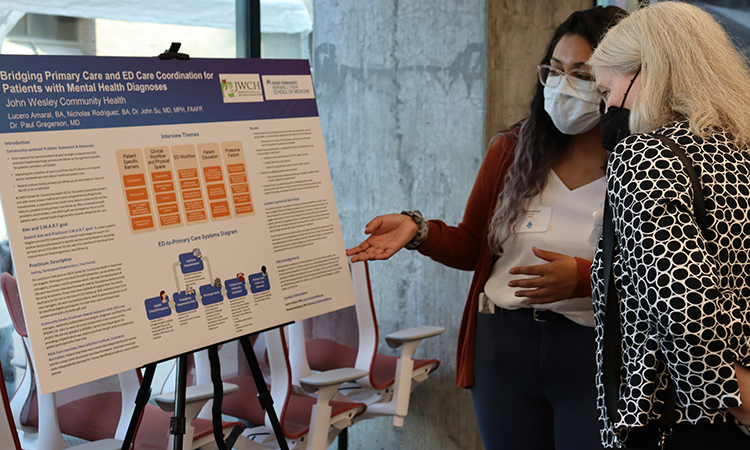
The Kaiser Permanente Bernard J. Tyson School of Medicine (KPSOM) Service-Learning Course in collaboration with the school’s Department of Health Systems Science, Office of Community Engagement, and community partners—hosted a celebration on July 21, 2022, at the school’s Medical Education Building to commemorate the Class of 2024 cohort’s completion of community-based learning experiences. The inaugural event marked the first time KPSOM students achieved this major milestone since the medical school opened its doors in July 2020.
“We are thrilled to celebrate our very first cohort of students who have had an opportunity to take part in a program aimed at improving the health of communities,” said Lori Carter-Edwards, PhD, MPH, KPSOM Assistant Dean for Community Engagement. “Through interactions with our community partners, students have become more knowledgeable, credible, and trusted partners to the patients, communities, and community partners with whom they are working. Further, their deep engagement at these facilities has hopefully equipped them with skills necessary to be more well-rounded medical students, capable of understanding both barriers and facilitators to health and health equity in the communities they serve.”