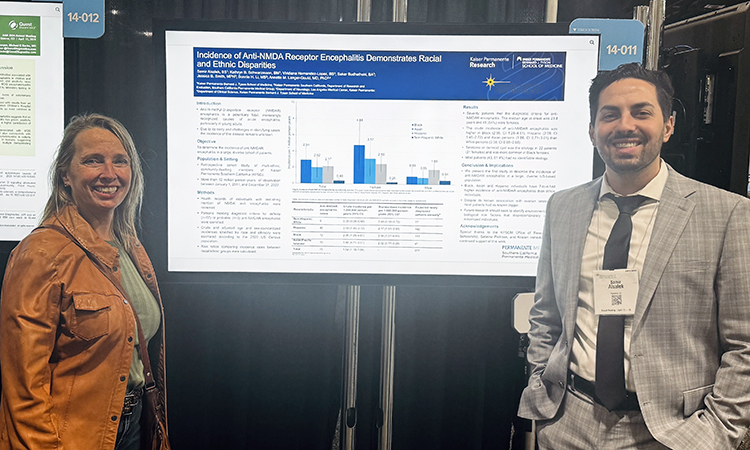
Kaiser Permanente Bernard J. Tyson School of Medicine student Samir Alsalek is first author of the study, Racial and Ethnic Disparities in Incidence of Anti-NMDA Receptor Encephalitis, which was presented during the 2024 American Academy of Neurology meeting in Denver, Colorado, in April. Utilizing data from a diverse spectrum of patient populations from the Kaiser Permanente Southern California healthcare system, the study examines Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis, a potentially fatal, increasingly recognized cause of acute encephalitis, and attempts to address gaps in knowledge where prior studies have failed to estimate the disease’s incidence or examine racial/ethnic differences. Alsalek collaborated in the research with the project mentor, Annette Langer-Gould, MD, PhD, KPSOM Clinical Professor of Clinical Science; KPSOM students Kathryn Schwarzmann, Sakar Budhathoki, and Viridiana Hernandez-Lopez; and Kaiser Permanente research assistants Jessica Smith and Bonnie Li.
The following interview with Samir Alsalek was lightly edited for clarity and length.
To begin, what is Anti-NMDA Receptor Encephalitis and how did you choose to make it the focus of your study?
Encephalitis is a generic term for brain tissue inflammation, and there are multiple types. Its etiologies include viral and autoimmune, among others. For example, the type that we studied belongs to the autoimmune family of encephalitides. There are multiple types of autoimmune encephalitis; this specific type occurs when the body produces antibodies to a specific receptor in the brain, NMDA, hence the name Anti-NMDA Receptor Encephalitis. It first came to my attention through Dr. Langer-Gould, who I was beginning to work with as my research mentor. We talked about multiple possible projects and Anti-NMDA Receptor Encephalitis came up. The fact that there were currently no incidence estimates for this disease, although it's becoming increasingly more recognized and diagnosed, made this a particularly interesting project. We identified a gap in knowledge about this disease and saw an opportunity to fill that gap using the Kaiser Permanente data. Kaiser Permanente’s unique structure as a large integrated health system means that its members, specifically within the Kaiser Permanente Southern California network, can be considered a population that is multiethnic, multiracial, and representative of the broader U.S. population, with few small exceptions.
How did you go about accessing the data that you needed to conduct this study?
All studies that utilize Kaiser Permanente data have to be approved by the Institutional Review Board (IRB). Following the process through the IRB, we got approval to access the data. The next thing we did was search the charts of all Kaiser Permanente Southern California members over the course of our study duration for the keywords “encephalitis” and “NMDA.” The purpose of that search was to identify suspected cases broadly. This was done because there's currently no International Classification of Disease (ICD) code for the disease; ICD codes are standardized codes assigned to conditions and diseases to allow for their quick identification in the electronic medical record virtually anywhere in the world. Unfortunately, as this disease does not have an ICD code yet, which is what made case identification challenging in the past and why we didn’t have incidence estimates to date.
What was the study duration and sample size?
We measure it in something called person-years, which is a product of the number of people in the database and the duration which they were part of the database. When looking at that, we included over 10 million person-years of observation. The period that we studied was between 2011 and 2022.