Throughout the course students engage with four different types of narratives. These narratives will be important to their work as a doctor some day and are deeply connected to how they approach patient care in the future. “EID is foundational to what it means to be a caring, person-centered physician,” said Dr. Lawson. “I believe the best physicians see their patients as people, and therefore must take into account how broader social systems and structures affect, often inequitably, a person’s lived experience, their health, and treatment options.”
At the start of the course, one might wonder how discussing works of art could possibly help develop core skills needed for doctoring.
“Yes, [in medical school] we’re giving you a whole lot of knowledge about how the body works—anatomy, biochemistry, pharmacology, we’re teaching you clinical skills, we’re teaching you evidence-based medicine,” said Dr. Gowda. “But it’s your powers of imagination that is going to allow you to then go into the world to observe the problems that you’re seeing and generate solutions for those problems in your clinic, in your community, maybe even nationally or globally. The solutions for today’s problems don’t come from an algorithm. They have to be generated through your own powers of imagination, collaboration, and problem-solving.”
First, students delve into this work by observing stock narratives. These are stories in society that might maintain social structures and consider individuals whose voices and perspectives are not being heard. “Because this work is so steeped in pain and loss and inequity, I find it critical for us to find and center those pockets of hope and joy,” said Dr. Lawson. “Without them, it is hard for students to see how they can make an impact. How even the briefest conversation can have a lasting impact on them and on the people and communities they engage with.”
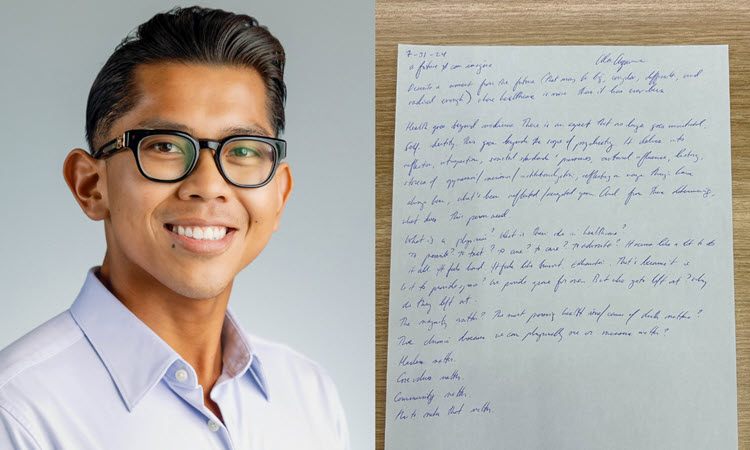
Next, they look at concealed narratives. For this session students are encouraged to look at different creative works while also examining their own lives and clinical settings. They are then asked to think about those in their clinical settings whose stories are not being heard.
“We have deep conversations about power and how that affects a person’s voice,” said Dr. Gowda. “What are the consequences of the patient's preferences, values, and perspectives not being heard in decisions about their care plan?”
This is part of the reason why the third session of the narrative medicine work is centered on resistance narratives. The students get to explore communities around Los Angeles that have advocated for better healthcare and change within their own communities. Through these experiences students are asked to think about what stories help us to understand when people have fought for change and why.