When the COVID-19 pandemic emerged in the United States last spring, medical schools had to quickly reimagine how to train their students, including how to teach foundational subjects such as anatomical science.
Last July, the Kaiser Permanente Bernard J. Tyson School of Medicine (KPSOM) adopted a hybrid model of instruction for its 50-member inaugural class. The school’s Anatomy Resource Center (ARC) made it possible to offer both a hands-on and virtual environment for learning about the human body.
The ARC is central to the school’s modern approach to teaching anatomical science. KPSOM utilizes a multi-modal method for instruction and assessment in gross anatomy, which includes microscopic anatomy or histology, embryology, and clinical anatomy. Rather than a standalone course, anatomy is a longitudinal discipline taught throughout the curriculum and integrated into a variety of Human Systems-based courses.
The school employs six full-body pre-dissected human cadavers (three male and three female) preserved by plastination, instead of traditional lightly embalmed cadaveric dissection. There are multiple specimens of all the organs, limbs, and regions at the ARC as well, to be inspected independently and separate from the full cadavers. Unlike traditional cadavers which can generally only be used for a few weeks and are destroyed as they are dissected, plastinated specimens can last for many years and are available for the entirety of the medical school experience.
“Our students gain an appreciation for normal human variation. You cannot get this from an atlas or a single cadaver,” said Dr. Jose Barral, Professor and Chair of the Department of Biomedical Science. “It also allows students to interact physically with the anatomy in question and explore it easily by direct visual and tactile inspection.”
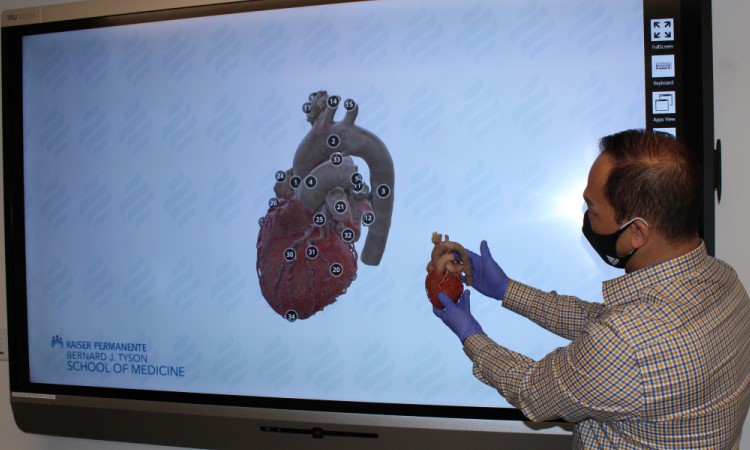
Computer-assisted software, augmented reality, and interactive diagnostic tools, including simulated ultrasound devices and mannequins, are also used, creating a dynamic learning environment at the center. Students often work together at touch-interface workstations that allow them to visualize and interact with many human structures in 3D and cross-sectional views of the body.
First-year student Christian Mark Agatep was curious about the school’s approach to teaching anatomy through plastinated cadavers and touch-screen apps.
“Learning anatomy by way of dissection of cadavers has always felt like a sacred rite of passage in medical school, as we ruminate on the idea of life and death and building relationships with our future patients,” he said. “However, during my interview at KPSOM, we were introduced to the wonderful technology and plastinated cadavers in the ARC and I was instantly sold.”
For classmate Kelly Shriver, the school’s patient-centered approach to teaching anatomy was one of the main reasons she chose to study at KPSOM.
“I’m certainly fascinated with the body and how it all works, but I’m interested in this in the service of becoming a physician who can appropriately treat my patients,” she said. “The feeling of patient-centered learning has carried through my experience at the ARC and in anatomy sessions in class where we explore anatomy through the lens of how it affects actual people ─ which are you more likely to tear? Why is it vulnerable? Can we prevent the injury? How do we fix it?”
Throughout the pandemic, students were able to schedule “office hours” to safely review materials and interact with the plastinates with other faculty and students in the center, which is run by two dedicated full-time staff members.
When in-person operations at the school were temporarily suspended, faculty members created both livestream and videotaped instruction from the ARC. Plastinates could also be used in small group classrooms throughout the Medical Education Building when group meetings were not advisable.
The school recently purchased two 3D scanners for the center, which are being used to create multidimensional models, labeled by anatomy experts, of the entire plastinated collection. The 3D scans are accessed through a web browser, allowing students to view them anytime on a computer or mobile device.
“If students are doing a knee injection at a clinic, they can bring the scan of a dissected knee up on their iPhone and review it right there and then,” said Barral. “Afterwards, when they come to school and the ARC, they can inspect the real, physical knee to further consolidate their learning.”